Free Upgrades, Unfortunately
By Elsa Youngsteadt
Tuberculosis bacterium becomes drug-resistant without penalty
Tuberculosis bacterium becomes drug-resistant without penalty

DOI: 10.1511/2006.62.502
Contrary to infectious-disease dogma, the mutations that enable bacteria to resist antibiotics do not always result in weaker strains, according to a study published in the June 30 issue of the journal Science. This is bad news for public-health efforts, especially because the germ in question is the tuberculosis-causing Mycobacterium tuberculosis, once the leading cause of death in the United States.
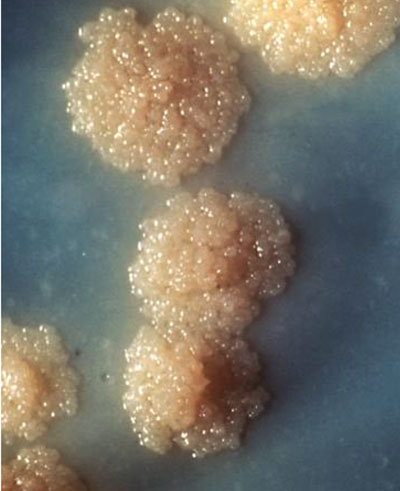
Photograph courtesy of Centers for Disease Control and Prevention/George Kubica.
Classic laboratory experiments once suggested that bacteria pay a price for antibiotic resistance—that resistant bacteria are weaker than their susceptible counterparts and should not spread through the human population when forced to compete with hardier strains.
But the new study, headed by scientists at Stanford University, has undermined this comforting conventional wisdom. It shows that in real human patients, tuberculosis bacteria can evolve resistance to antibiotics and still be just as aggressive as their susceptible ancestors.
"It's generally bad news for the world that some tuberculosis strains can get something for nothing," said Sebastien Gagneux, one of the lead authors of the study and a research associate at the Institute of Systems Biology. "Even though many drug-resistant strains are less hardy than susceptible strains, others evolve over the course of treatment and remain virulent."
M. tuberculosis has plagued humans throughout history. Improved public health brought the epidemic under control, and the advent of antibiotics in the 1940s seemed to ensure successful treatment. But the bacteria have adapted to nearly every drug used against them. With its recent resurgence, the disease now kills a person every 15 seconds, worldwide. Public-heath experts say the antibiotic-resistant strains may be around to stay. "Evolution is a powerful engine," says Peter Small, senior program officer of the Tuberculosis Global Health Program and contributing author of the Science paper.
Gagneux and coauthor Clara Davis Long of Stanford suspected that the lab studies underpinning the epidemiological credo might be missing the big picture. A human being is, after all, a very different environment than a culture plate. So Gagneux, Davis Long and their collaborators took a more thorough look at the cost of antibiotic resistance in tuberculosis bacteria, using not only the usual lab-generated strains, but also those sampled directly from human tuberculosis patients.
The investigators looked at the evolution of resistance to the drug rifampin, one of the preferred first-line treatments for the disease. Rifampin binds to the molecule that makes, or polymerizes, bacterial RNA. The drug disables the so-called polymerase molecule and prevents the crucial flow of information from DNA to RNA. Without RNA, bacteria can't make the proteins they need to survive. But simple mutations in the gene that encodes RNA polymerase can change its structure. The different shape decreases the drug's ability to bind and allows M. tuberculosis to persist in the face of antibiotic onslaught. Classic studies suggested that such a change would carry some cost, such as decreased efficiency of the polymerase molecule. Such a penalty would cause the mutants to grow more slowly than unmodified strains, thereby retarding the spread of the antibiotic-resistant mutation in the population.
Not so, according to the new study, which found that some resistant bugs are every bit as robust as unmodified strains. The Stanford group collected tuberculosis bacteria from the sputum of patients, first at the beginning of their infections, and a second time after some of those patients developed rifampin-resistant infections. The investigators then pitted the resistant strains against their susceptible counterparts in antibiotic-free competition assays. These tests force the two strains to compete for limited resources in a common culture flask, so the hardier bug should take over as the weaker one gets crowded out. Contrary to expectations, five of the ten resistant strains held their own in these tests, and one actually dominated its antibiotic-susceptible ancestor.
These results suggested that the evolutionary changes that lead to drug resistance occur differently in human patients and culture dishes. To confirm this conclusion, the scientists generated several rifampin-resistant strains in the lab, simply by exposing M. tuberculosis to growth media that contained a small amount of the drug. Each resistant strain that arose had a single mutation in the RNA-polymerase gene, and some of the changes were identical to those found in strains isolated from human patients. However, unlike the bacteria from the clinic, all the mutated laboratory strains were weaker than their susceptible progenitor. This part of the study parallels the methodology underpinning the conventional wisdom, and it highlights the difference between what goes on in the lab and what goes on in a human patient.
"Bacteria exist in heterogeneous populations of different strains. If you just look at lab-adapted strains, you won't get the right answer," Gagneux said. "By looking at clinical isolates, you find that some kind of selection is going on in patients that is different from what happens in a culture plate."
Although the laboratory mutants were less fit than their clinical counterparts, the cost of the lab-generated mutations was still related to their prevalence in clinical samples. The specific mutations that were least costly in the lab bacteria were the same ones that carried no cost for clinical strains and occurred most often in patients. The costliest mutations generated in the lab never turned up in a patient. In other words, "you don't see wimpy bugs in the real world," Small said.
Despite its grim conclusion that our old enemy is more versatile than we believed, the study also yielded some insights that may prove useful in the fight. "The good news is that some very simple in vitro competitive assays reflect the behavior of these bacteria in the real world," Small added. "Now we have a link between a pathogen's in vitro ecology and its epidemiology, and that link can be incorporated into predictive models. Laboratory data can tell us in advance whether a particular bug is a concern. We don't have to wait and see."
Just how clinical isolates outperform lab-generated strains with identical mutations remains a mystery. Some changes simply have a low cost to begin with, and, the study also found, the cost depends on the strain in which the mutation occurs. However, the real key is likely to be compensatory mutation—one or more additional changes, in the same RNA polymerase gene or in related genes, that make up for the diminished function caused by the original mutation. Gagneux is planning future studies to find these putative compensatory mutations and learn how they restore the performance of strains that acquire antibiotic-resistance mutations.
The authors don't want their study to fuel an alarmist panic. Indeed, the data don't call for it, says Bruce Levin, an expert on the evolution of antibiotic resistance at Emory University who was not involved with the study. Levin points out that "the spread of tuberculosis does not depend solely on the efficacy or lack of efficacy of antibiotics." He cites public-health practices and better nutrition as bulwarks against 19th-century-style epidemics.
However, the paper does highlight a sobering trend in human epidemiology. Drug-resistant bacteria are here to stay, even if society stopped abusing antibiotics right now. Furthermore, evolution doesn't just work on bacteria. Levin explains, "the drug-resistant mutations that aren't costly are the ones that will take over, not only in the bacteria responsible for tuberculosis but also in [organisms] responsible for other diseases."
Click "American Scientist" to access home page
American Scientist Comments and Discussion
To discuss our articles or comment on them, please share them and tag American Scientist on social media platforms. Here are links to our profiles on Twitter, Facebook, and LinkedIn.
If we re-share your post, we will moderate comments/discussion following our comments policy.