Routes of Resistance
By Robert Dorit
Our focus on using antibiotics to kill bacteria has blinded us to their diverse functions in the organisms that make these chemicals
Our focus on using antibiotics to kill bacteria has blinded us to their diverse functions in the organisms that make these chemicals

DOI: 10.1511/2009.76.29
Last year, some 50 million pounds of antibiotics were used in the United States, an amount that would correspond to roughly 5 tablespoons—or 75 doses—of antibiotics per person. In fact, much of this antibiotic—as much as 70 percent by some estimates—is being used not to treat infections, but instead to promote food production, as antibiotics have become a key ingredient in the American food chain. We are, in short, marinating the living world in antibiotics.
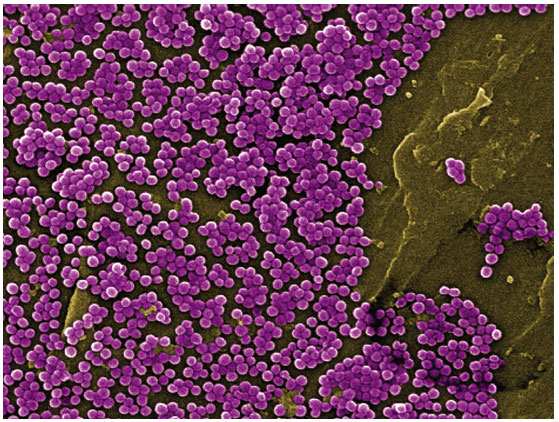
Image courtesy of CDC/Jeff Hageman, M.H.S, photo by Janice Haney Carr.
Against this backdrop, the emergence of antibiotic-resistant pathogenic bacteria can hardly come as a surprise. Antibiotics, after all, are used to suppress and kill bacteria, and bacteria, like every other living thing, have no greater evolutionary imperative than to stay alive. Our overuse of antibiotics methodically rewards any bacterium fortunate enough to carry a mutation that confers even slight resistance to the substance in its environment. The less-fortunate bacteria die, leaving behind empty ecological space for resistant strains to fill. Slowly and inexorably, we thus enrich the world with bacteria that now scoff at our attempts to control them.
It did not take long for antibiotic resistance to emerge once the drugs entered the arsenal of modern medicine. Penicillin, discovered in 1929, came into widespread use on the battlefield during World War II: Some 100 million doses were produced between 1943 and 1945. But even before the end of the war, the first penicillin-resistant strains of bacteria appeared. Over the next five decades, the pattern repeated numerous times. The discovery of every new antibiotic class created excitement by promising to bring bacterial infections to heel. Inevitably, however, the edge of this new tool for the treatment of infections became blunt with overuse as resistant strains grew common. The useful clinical life of new antibiotics, defined as the time between clinical introduction and the rise of resistant strains, is often no more than a matter of three to five years. Over the past decade, moreover, antibiotic resistance, once only a public-health concern, has morphed into a measurable cause of death. Conservatively, untreatable bacterial infections result in some 100,000 deaths per year in the United States. The early promise of the age of antibiotics—an end to infectious diseases—now seems absurdly naive.
But every day, in clinics and hospitals around the world, doctors are forced to administer antibiotics to clear up bacterial infections that threaten the lives of patients. And every day, the bacteria—both the pathogens we are targeting and the innocent bystanders that end up as collateral damage—respond by evolving mechanisms to resist the antibiotics. Each dose is a skirmish in a larger war. Yet, focused as we are on what we see as an epic battle between humans and pathogens, we forget that both antibiotics and antibiotic resistance have been part of the microbial world for the past 3 billion years. Yes, the widespread use of antibiotics to combat infections has had profound implications for the evolution of infectious disease, but it is a mere blip in the history of the microbial world.
Four out of five antibiotics in use today are based on naturally occurring compounds produced by bacteria and fungi. The organisms that produce antibiotics have not, of course, been doing so over billions of years just so that we might discover them and put them to therapeutic use in the 21st century. So what are antibiotics doing for the organisms that produce them? The explanation most obvious to us, of course, is to see these compounds as part of the competitive arsenal of the bacteria that produce them. In this model, antibiotic-producing bacteria kill their competitors and make ecological space available for themselves and their genetic kin. Seen this way, antibiotics in microbial ecosystems and antibiotics in the clinic do one and the same thing: kill bacteria.
To be sure, naturally produced antibiotics in intact microbial ecosystems enable producing strains to kill other bacteria. Some antibiotics, such as a class of proteins called the bacteriocins, are not subtle: A single molecule entering a target cell will kill it. These molecules are designed to kill and nothing more. But the concentrations of many other antibiotics in natural ecosystems seem consistently too low to kill surrounding organisms effectively. Why would bacteria bother to produce antibiotics—which are expensive molecules to synthesize—at concentrations too low to reap the benefits? It now appears that at lower concentrations, antibiotics may well, to the bacteria, mean something utterly different than they do at the massive concentrations encountered in the clinic. In their original context, antibiotics may not be killers at all, but instead messengers enabling cell-to-cell communication both within and across bacterial species boundaries.
Researchers such as Fernando Baquero and Jose L. Martinez of the National Center for Biotechnology in Madrid, and Julian Davies of the University of British Columbia, among others, have begun to articulate a radically different perspective on the role played by the now-mislabeled “antibiotics.” Far from being just stone-cold killers, naturally occurring antibiotics appear to be part of the vocabulary of bacteria, words in the nuanced language of this world unseen by humans. Like language, antibiotics are capable of conveying multiple meanings to different recipients.
At sublethal concentrations, antibiotics can have profound and unexpected effects on surrounding cells. Several different antibiotics, when present at a small fraction (less than 1 percent) of their lethal concentration, coordinate the expression of whole sets of genes in bacteria that sense the antibiotic. These coordinated responses are not simply the molecular expression of panic (the aptly named “SOS response”) expected when an antibiotic is present. The signal may, for instance, induce Pseudomonas aeruginosa bacteria to develop into a bacterial biofilm—an architecturally complex, surface-bound conglomeration of cells—which, regrettably, makes bacteria much less sensitive to antibiotics in clinical settings. In another irony, low concentrations of antibiotic appear to upregulate the expression of a suite of genes responsible for increased virulence, in effect transforming a benign bacterium into a pathogen. These and other examples, in short, suggest that antibiotics may be far more than just toxic substances designed to kill all bacteria within range. And in the latest of many surprises, George M. Church of Harvard Medical School and his colleagues have isolated hundreds of soil bacteria able to subsist on antibiotics as their sole source of nutrition. This is not resistance but rather downright insolence, as these bacteria think of antibiotics not as threatening molecules, but instead as food.
Our ability to understand the origin and role of antibiotics has, in effect, been hindered by the uses to which we put them. In a fit of intellectual narcissism, we assume that if we use them in clinical settings to kill bacteria, that must be what they evolved for. However, when we recast them in a subtler role as agents of competition, and also as regulators and communicators in the bacterial world, we can view their lethal (and thus, for us, salutary) effects in a different light. It is when we administer doses of antibiotics that are orders of magnitude greater than those encountered in nature that a subtle, modulated signal is transformed into a deafening, and increasingly deadly, roar.
If antibiotics are part of the whispered conversations of the microbial world, what then should we make of antibiotic resistance? The last 65 years of clinical antibiotic use have exposed a dizzying array of mechanisms that bacteria use to survive the presence of toxic antibiotic concentrations. The diversity and complexity of these mechanisms—enzymes that chemically disable antibiotics, shape-shifting targets that prevent antibiotics from binding, complex pumps that eject the antibiotic from the target cell—have raised an obvious evolutionary question: Where do these mechanisms come from? Part of the answer, unsurprisingly, is self-defense. Many of the bacteria that produce antibiotics also harbor mechanisms that make themselves impervious to that antibiotic compound. In the case of the lethal protein antibiotics discussed previously, the bacteriocins, producer bacteria also synthesize a second protein that pairs up with the antibiotic, rendering it inactive until it reaches its target.
In the classic militaristic interpretation, antibiotics exist to target competitors, and resistance genes evolve to protect producers. But here again, we might do well to remember that massive concentrations of antibiotics used in clinical settings, and the consequences of such massive use, may be obscuring subtler phenomena in the microbial world. A second effect, which I will call the Pete Townshend effect, may also underlie some of the evolution of resistance. In this scenario, antibiotics are playing their signaling role, but the levels of this signal molecule are so high in and around the producing cell that they will cause unintended damage as a byproduct of their high concentration. Resistance evolves in producer strains to protect them from the damaging consequences of overwhelming signal strength. As the antibiotic diffuses away from the producer, its concentration declines. The antibiotic loses its lethality and regains its signaling function. If antibiotics have multiple meanings, resistance too must mean more than one thing.
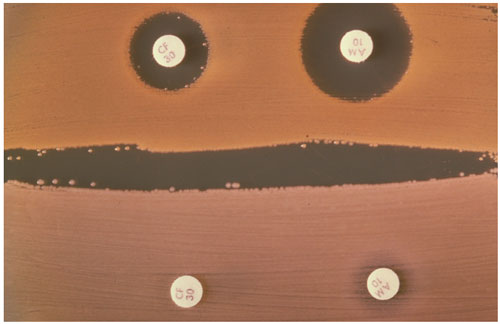
Image courtesy of CDC/Dr. J. J. Farmer.
Our ability to examine the genomes of both culturable and unculturable organisms has changed the way we look at the origin of antibiotic resistance mechanisms. Resistance is everywhere, and we don’t always know why. We now realize, for example, that the bacteria in a gram of soil harbor hundreds of different genes that can, in the right setting, contribute to resistance. For instance, work by Gerard D. Wright of McMaster University and others, reveals that bacteria in the soil already harbor the rudiments of resistance to all known antibiotics, including entirely synthetic antibiotics with no counterpart in the natural world. Virtually every bacterial cell in these environmental samples is, on average, resistant to eight antibiotics.
The collection of mechanisms responsible for resistance in these soil bacteria has come to be called the “environmental resistome” (as it rhymes, as everything must nowadays, with “genome”). The samples used to investigate the resistome are not ones where clinical strains selected for resistance might be congregating (although wastewater streams from hospitals and water treatment plants in large cities harbor their own impressive collection of clinic-selected resistant strains). Instead, virtually every sample used has a stable microbial ecosystem that has never been exposed to clinical levels of antibiotics and has not been in contact with resistant clinical bacterial cultures. Nonetheless, every one of the samples harbors a vast repository of resistance genes.
This environmental resistome provides a glimpse of the raw materials that clinical pathogens have accessed in the antibiotic age. What is sobering about the discovery of the resistome is the revelation that the microbial world already possesses a functional arsenal of defenses against the antibiotics we develop for clinical use. The resistome also demands a subtle, but critical, change in our perspective on resistance: Many of the mechanisms involved in so-called resistance may be playing other critical roles in cells coexisting peacefully with their neighbors. If antibiotics at sublethal doses really are signal molecules, perhaps resistance is really a signal modulator, altering the meaning and modifying the effects of the message on the recipient cell. Once again, the context in which we usually first encounter resistance mechanisms—in clinical infections as they become insensitive to therapeutic doses of antibiotics—may be obscuring the many roles these mechanisms play in the microbial world.
We cannot lose sight of how profoundly 50 million pounds of annual antibiotic use impacts the microbial world. The widespread use of antibiotics has created a black market for antibiotic resistance mechanisms where bacteria poach ready-made shortcuts to resistance: It has enhanced and rewarded the evolution of a vast network that allows for the transfer of resistance along nongenealogical lines. These mechanisms of horizontal transfer now connect the extensive environmental resistome with any pathogen (or commensal bacterium) exposed to clinical concentrations of antibiotic. As a result, bacteria in the presence of potentially lethal concentrations of antibiotics no longer face the daunting evolutionary challenge of remaining alive while they and their descendants cobble together resistance one point mutation at a time. Instead, fully functional resistance located on moveable genetic elements can now be acquired by swapping with other bacteria, or by taking such elements up directly from the environment.
To make matters more challenging, many of these ready-made resistance elements are packaged as a set. Multiple genes encoding resistance to multiple antibiotics now travel as a team (up to 74 different resistances have been found to occur together). The ubiquitous presence of human-administered antibiotics in the environment selects strongly for bacteria that are able to acquire these resistance packs, and may also be selecting for the evolution of increasingly mobile and promiscuous elements equipped with increasingly diverse arrays of resistances. As mobile elements, their Darwinian imperative is to make and move copies of themselves, and that in turn may depend on their ability to keep their host bacteria alive in a sea of antibiotics.
Many forces—social, economic and medical—propel excessive antibiotic use. An expanded perspective on the role of antibiotics and resistance in no way contradicts the urgent need to reduce antibiotic consumption. Our current behavior, moreover, drowns out the subtle melody unfolding in microbial ecosystems and superimposes the deafening roar of therapeutic antibiotics and increasingly resistant pathogens in its place. We can hope that new antibiotics will continue to be developed and broadly prescribed, buying us a few more years. We can keep doing what we have always done, and hope we can reach a stalemate with ever more-aggressive bacterial pathogens. Or we can instead start paying more attention to what microbial ecosystems have to teach us, acknowledging the lessons that have always been embedded in a gram of soil. Our relationship to the unseen world extends far beyond pathogens and our efforts to combat them. We can, if we put our minds to it, begin to see a world in a grain of sand.
Click "American Scientist" to access home page
American Scientist Comments and Discussion
To discuss our articles or comment on them, please share them and tag American Scientist on social media platforms. Here are links to our profiles on Twitter, Facebook, and LinkedIn.
If we re-share your post, we will moderate comments/discussion following our comments policy.