Suffocating from Medical Bias
By Gilda Ann Barabino, Harriet B. Nembhard
A systems engineering approach to equitable health care solutions
A systems engineering approach to equitable health care solutions

The United States is in the midst of a public health crisis, reeling from two serious pandemics: COVID-19 and systemic racism. Everyone is familiar with the impact of the virus. The categorization of racism as a pandemic may seem less obvious, but when viewed through the lens of systems engineering, racism in the American health care system can be seen to contain tightly linked problems of medicine, technology, design, leadership, and ethics. The intersections are myriad, bound in racial disparities that pervade all aspects of life, including such basic functions as the ability to breathe.

© World Health Organization/Ismail Taxta
For Black people and other racially minoritized groups, the health care system—which should provide equitable treatment and care—is tainted by disparate access, poor quality of care, unequal outcomes, and distrust between individuals and health care providers. The extent to which racial biases lead to health care disparities is influenced by demographics; environmental, social, and economic conditions; and policies and practices that pervade all aspects of life.
Our research takes a systems engineering approach to examining racism and health care, with particular attention on the disproportionate effect of health crises on Black people. Systems engineering is an interdisciplinary field of engineering that focuses on the design, operations, and management of complex systems; it considers the technical and business needs of all stakeholders in a system in order to provide quality products and outcomes over a long-range life cycle. The broad scope of this approach allows researchers to tackle large problems without losing sight of the details. The goal of our work is to identify the racial biases inherent in the health care system, and suggest solutions toward a better and more equitable future. Engineering and technology have long played an important role in health care, from the design and manufacture of early medical devices to the current deployment of electronic medical records and artificial intelligence for health screening. However, biased algorithms and technologies, along with a lack of diverse innovators, mean that not all people benefit equally from these advances.
To address the racial pandemic in health care, we need to recognize that engineering and technology are influenced by society and operate within the context of social and political forces. Even neutral-seeming medical devices or drug protocols can contain harmful, embedded racial biases. Those biases must be acknowledged and addressed if we are to create a more humane and effective system of health care.
The system of racial disadvantage across housing, schooling, employment, wealth, and health is well documented. Social scientist David R. Williams of Harvard University, who studies social influences on health, has described this societal system as the ”house that racism built,” noting how the system of racism (with institutional, cultural, and individual discrimination components) is impacted by social forces with multiple pathways to undermine health. To better understand interrelated racial disparities across multiple domains, University of Washington sociologist Barbara Reskin describes race discrimination as a system of dynamically related subsystems in which disparities systematically favor certain groups and are mutually reinforcing. Where someone lives can dictate where they are schooled, which can in turn constrain employment opportunities; it can also determine whether they have access to quality health care or are exposed to environmental elements that are detrimental to their health.
Protecting Black lives means protecting Black breath, which means addressing the discriminatory design in medical devices and more broadly in the health care system.
For Black people, racism and its relationship with breathing have a long history that was brought into sharp focus in 2020 by the murder of George Floyd by suffocation, and by the COVID-19 pandemic that has seen disproportionate numbers of Black people succumbing to respiratory disease. Gabriel O. Apata (an independent scholar of philosophy, sociology, and the African diaspora) explains in his 2020 article “I Can’t Breathe” the ways in which racism targets breathing itself, with “social air” representing freedom and suffocation representing its negation. Apata’s suffocation theory describes racial suffocation as the slow, methodical, and invisible process by which racially unjust policies, practices, and behaviors combined with the lack of access to resources and opportunities systematically squeeze the social air breathed by Black people, leading to their deaths.
The normal respiration rate for a healthy adult who has no difficulty breathing is 12 to 20 breaths per minute while at rest. A device called a spirometer measures the amount of air a person can breathe in a single deep breath as well as the rate of that breath. The spirometer has a long and sordid history in the subjugation of Black people. Lundy Braun, a professor of medical science and Africana studies at Brown University, has shown how this device has adversely shaped medical research and practice for many decades. The legacy of slavery as embodied by disparate treatment and health outcomes for Black people takes many forms, one root of which is to devalue Black lives—often through misrepresented biological differences between Black and white people.
Braun found that in the mid-19th century, plantation physician and slaveholder Samuel Cartwright used a spirometer to compare the lung capacities of enslaved Black people with those of white people. His findings perpetuated the misconception that Black people have lower lung capacity than white people, which provided support for racially defined inferiority. This fallacy endures as race continues to be used out of context in medical measurements, and most modern spirometers still include a race-based lung function algorithm that assumes lower lung capacity for people of color, thereby resulting in undertreatment of breathing conditions in people of color.
When oxygen saturation is below 90 percent, there is danger to vital organs such as the heart, brain, lungs, and kidneys. The ubiquitous fingertip pulse oximeter, which measures how much oxygen is making it into the blood, does not reliably work on people with darker skin. Since the population drawn upon for the development of the pulse oximeter was not racially diverse (a design flaw) and measurement of light transmitted through skin can vary with skin tone, discrepancies in readings for Black people are not surprising. Multiple studies, including a 2020 paper in the New England Journal of Medicine by Michael Sjoding (assistant professor of pulmonary and critical care medicine at the University of Michigan Medical School) and his colleagues, show that fingertip pulse oximeters produce biased results that make it more likely that medical providers will underdiagnose occult hypoxemia in Black patients.
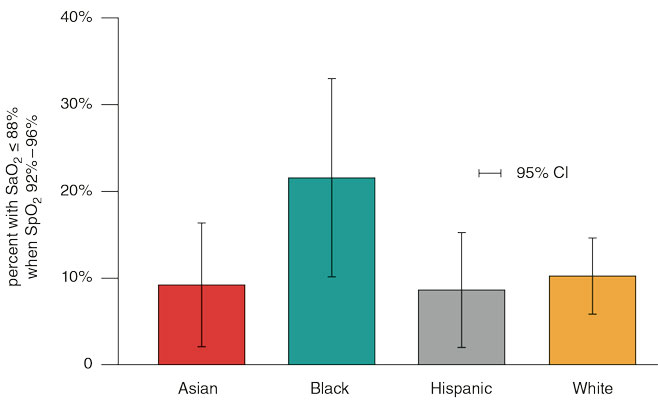
Adapted from V. S. M. Valbuena, et al. 2022.
Given that oxygen is a frequently administered medical therapy, there are widespread consequences of this racial bias. Philosophers Shen-yi Liao of the University of Puget Sound and Vanessa Carbonell of the University of Cincinnati have used spirometers and pulse oximeters as case studies to demonstrate how racism is encoded in medical devices. They argue that these devices materialize oppression, meaning that the tools’ inherent racial biases produce tangible harm based on racial difference, thereby perpetuating an unjust hegemonic system. The measurement of breath and oxygen is fundamental to the care of all patients, and biased readings can have life-threatening implications for Black patients with a range of medical issues. For example, most patients with sickle cell anemia develop abnormal pulmonary function, which is characterized by airway obstruction, restrictive lung disease, and hypoxemia. Pulmonary complications of the disease, which turn fatal in a large proportion of patients, may be underappreciated by health care providers. Poor understanding of health complications for Black people has many causes, including false assumptions about biological differences, racial biases in the designs of medical devices, and researchers and clinicians ignoring societal factors.
COVID-19 is also having disproportionate impacts on Black and brown populations. A 2021 study led by National Cancer Institute epidemiologist Meredith S. Shiels found that in 2020 more than twice as many Black, American Indian, Alaska Native, and Latino men and women than white and Asian men and women had died of COVID-19. Biased breathing measurements may have contributed to this disproportionate outcome because COVID-19 can cause lung complications such as pneumonia or acute respiratory distress syndrome (ARDS). Sepsis, another possible complication of COVID-19, can also cause lasting harm to the lungs.
With these adverse outcomes in the balance, health care providers, engineers, and device designers ought to take greater action to fight discriminatory design. There is nothing more fundamental to life than taking a breath. Protecting Black lives means protecting Black breath, which means addressing the discriminatory design in medical devices, and more broadly in the health care system. For example, Ziad Obermeyer at the University of California, Berkeley, School of Public Health and his colleagues have demonstrated racial bias in algorithms used by health care systems; those algorithms assign lower risk scores to Black people, on average, leading to an underestimation of their health care needs.
The question becomes what practices, interventions, and resolutions will help to achieve equitable health care for all people. Achuta Kadambi, leader of the Visual Machines Group at the University of California, Los Angeles, describes a framework that identifies three ways that racial and gender bias can permeate medical devices—physical bias, interpretation bias, and computational bias—and argues that fairness should be considered equally important as effectiveness when evaluating new technology. All three types of biases are demonstrated in the technologies used to measure breath: the pulse oximeter is an example of physical bias; the spirometer is an example of interpretation bias; and health care algorithms are an example of computational bias.
Our work on complex systems and systems thinking provides useful approaches to studying the dynamic cause and effect of racism in health care. The word system in an engineering context means interrelated parts or components that cooperate in some way. In such systems, there is a need to focus on the interactions between components.
The complexity of the American health care system has led to layers of crises in safety, quality, cost, and access. Moreover, as health care providers gain experience and seek to make individual improvements, localized patterns of behavior in patient care emerge. There is no single point of control, and no one is “in charge.” Consequently, the health care providers within this complex system can typically be influenced more than they can be controlled.
Gilda A. Barabino and Harriet B. Nembhard
Applying systems thinking to the multifaceted American health care system ensures that the larger goal of fair and equitable care does not get lost as individual stakeholders address their specific areas of expertise. It is a holistic approach to analysis that focuses on how parts of a system interrelate over time and how they work within the context of larger systems.
As systems thinkers, engineers are well positioned to apply a systems approach to derive solutions to health disparities stemming from racism. We have been incorporating some of these connections into engineering education. But we can do more.
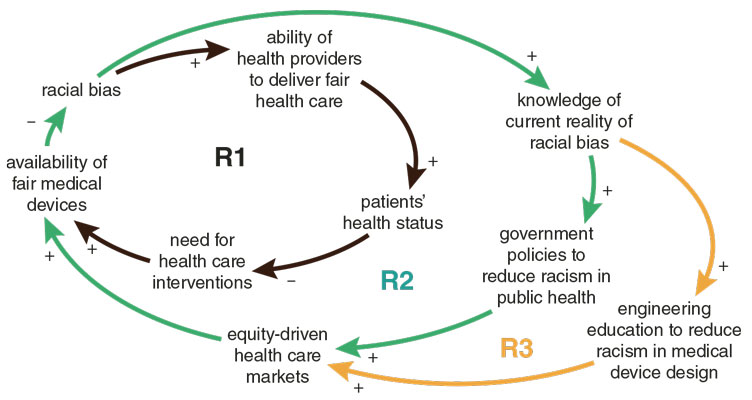
A systems thinking causal loop diagram provides an overview of how racial bias can be influenced within the complex system of health care (see figure above). The innermost reinforcing loop shows how the availability of fair medical devices affects the ability of health care providers to deliver fair health care, and thus patients’ resulting health status. The middle reinforcing loop shows how knowledge of racial bias, equity-driven health care markets, and government policies to fight racism add to the availability of fair medical devices. For example, last year the U.S. Food and Drug Administration released its “Artificial Intelligence/Machine Learning-Based Software as a Medical Device Action Plan,” in which the agency commits to supporting efforts to evaluate and improve the use of AI in medical devices with the goal of identifying and eliminating bias.
The outermost reinforcing loop conceptualizes the role and importance of engineering education. Engineering programs train their students in the systems thinking necessary to approach large and complex problems without losing sight of the big picture. Nearly every disciplinary area in engineering touches on health care, and biomedical engineers in particular are trained to combine a systems perspective with an understanding of the intricacies of health care.
As systems thinkers, engineers are well positioned to apply a systems approach to derive solutions to health disparities stemming from racism.
It is typical that biomedical engineering students have foundational courses in biomaterials, biomechanics, and bioinstrumentation that include training on modeling, acquisition, and analysis of data collected from living systems, as well as courses on medical device design fundamentals and prototyping, often culminating in a yearlong senior design capstone project. There are opportunities in these courses and others throughout the engineering curriculum to improve pedagogy and promote inclusive practices to reduce racism in design.
For example, students should be trained in the Societal Readiness Level, an expansive framework that provides a nine-stage scale for assessing the readiness of a product or innovation to be integrated into society. These frameworks need to be incorporated into the way we design and assess medical devices. Such work is also in alignment with the Accreditation Board for Engineering and Technology’s principles of diversity and inclusion, which state that these efforts to improve equity and representation are critical to innovation.
Moreover, we have the opportunity to ensure that engineering students are working in broadly interdisciplinary teams. These teams can and should include numerous parties: public health students and faculty members to understand how racism can affect health; anthropology and history colleagues to bring context to how medical oppression has impacted people; and medicine and nursing colleagues to bring awareness of patients’ lived experiences and how they are affected by the end designs of devices and systems. This convergent approach will support a network of embracing and transmitting systems of thinking about equity in health care.
The critical work ahead of us in engineering education is to enhance understanding of the causal relationships in American heath care, as well as the increasingly vast research that is expanding our knowledge of racism as a health determinant. Then we must collaborate to use that knowledge to create a better future, where medical devices and the provision of health care are more equitable for all.
Click "American Scientist" to access home page
American Scientist Comments and Discussion
To discuss our articles or comment on them, please share them and tag American Scientist on social media platforms. Here are links to our profiles on Twitter, Facebook, and LinkedIn.
If we re-share your post, we will moderate comments/discussion following our comments policy.