When Pigs Save Lives
By Haley Alexander
Scientists have made strides towards using porcine organs in transplants with the aid of recently deceased human recipients.
August 7, 2024
Biology Medicine Genetics
A person living with end-stage heart failure, who’s been told that they have been matched with a donor, experiences a huge range of emotions. “I don’t think anybody honestly understands that aspect of what it means to have a failing organ, and every day thinking ‘if I don’t get transplanted, I’m going to die.’ But also, they have the burden of thinking ‘the only way I’m going to get transplanted is, somebody else has to die.’ Some patients get very emotional, they feel for the other person and their families,” says Nader Moazami, cardiothoracic surgeon and chief of the division of heart and lung transplantation at New York University. However, the patients who receive transplants are the lucky ones: Around 50,000 people worldwide need heart transplants, but each year, only about 6,000 are performed. To close this gap, Moazami and his colleagues are working to advance a procedure called xenotransplantation, in which organs from nonhuman animals are used to replace failing human ones.
Research into xenotransplantation extends back some time. In the 17th century, practitioners attempted blood transfusions and skin grafts from animals to humans. In 1984, an historic xenotransplantation procedure using a baboon's heart was performed on one-month-old Stephanie Fae Beauclair, also called Baby Fae, who survived 21 days. Use of pig hearts was considered from the late 1980s, but in 1997, pig organ xenotransplantation was banned worldwide because of worries that a pig virus called porcine endogenous retrovirus (PERV) could be transmitted to humans. However, as studies progressed, it was concluded that this virus could not produce infectious particles in other species. A big leap forward in xenotransplantation came with the advent of gene editing, which could knock out genes that cause rejection, or add in genes that make an organ appear more humanlike to the immune system. Now, pig hearts that have had 10 genes edited are available.
To more safely study the human body’s response to these genetically modified pig hearts, Moazami and his colleagues developed protocols for transplanting them into decedents, people on life support with no brain function activity, who had previously consented to organ donation. Sometimes organs from such patients are not viable for donation, Moazami explains, and in such cases, the families are approached to see if they will donate the body for research. “These experiments were designed to only last for three days because keeping all these systems going in the patient for a long time is very difficult,” he says, “but also realizing that the decedents are the loved ones of someone who decided to donate their body to science, and their wishes for their body to be cremated or buried have to be respected with the same dignity as any other individual who passes away.”
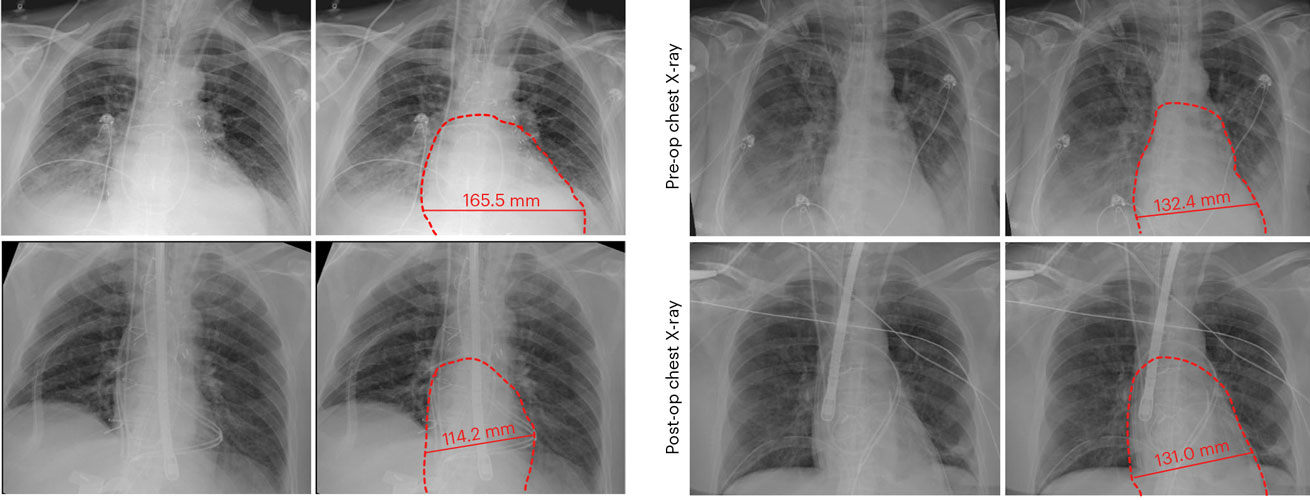
N. Moazami, et al., 2023, Nature Medicine 29:1989; top image: J. Boulet, et al., 2022 JACC: Basic to Translational Medicine 7:716; CC-BY-NC-ND 4.0.
The team was able to perform two transplants of genetically modified pig hearts into decedents. First, the heart is transported to the hospital after being preserved and submerged in an ice-cold solution. As soon as the transplant is finished, and the flow of warm, oxygenated blood flows into the heart cells, they automatically begin to contract. The first recipient, on June 16, 2022, was a 72-year-old man who had previously had heart failure and coronary artery bypass graft surgery. The pig donor was a male weighing 70 kilograms. Unfortunately, during the study, this patient's cardiac function declined because the donor heart was a little small. The second patient was a 64-year-old woman who underwent surgery on July 6, 2022. She previously had received two standard organ transplants. Her pig donor was a male weighing 69 kilograms. Luckily, the donor heart fit this patient perfectly. From these two cases, Moazami and his team were able to rule out any signs of cellular or antibody-mediated rejection. And there was no evidence of infectious disease transmission from one species to the other. “That moment when we saw the pig heart work, and work so well, the entire room was exhilarated by the feeling that maybe we can make this work, maybe we can get to the point in our lifetimes when thousands of people who die because they don’t have organs available, could be saved,” Moazami said. “It brings us a lot of encouragement that maybe it is possible that we’re at the brink of a timepoint where nobody has to be saved by the virtue of somebody else dying.”
The process of gene modification of a pig heart starts with a common type of cell called a fibroblast, which then has genes removed or added. After that, the nucleus is removed from a pig egg. The fibroblast and the empty egg are then fused together, resulting in the creation of a cell that has genetically modified DNA. This cell then goes through several division cycles, and the multicellular egg is implanted into a mother pig. The genetic modification will then be expressed in the newborn pig. However, at this time, the modified baby is not able to create offspring with this gene modification. Each pig has to be produced individually to receive this editing.
Moazami emphasizes that there are still a lot of hurdles to clear before xenotransplantation can be clinically successful. At the time of this study, the supply of modified pig hearts was extremely limited, which forced the team to work with whatever was available. The supply of pig donors would need to be large enough to carefully match the heart size with the patient. “One of the reasons that the pig is chosen as the potential donor is that pigs have a huge variation in size,” says Moazami. “What we are doing now as a research project is that we are trying to see if, using different imaging modalities, we can actually chart the growth of the heart relative to the growth of the pig.” But production of genetically modified pigs would need to be scaled up, and issues of quickly transporting donor hearts to transplant facilities also would need to be streamlined.
In addition, Moazami says, this study only addressed immediate, or hyperacute, organ rejection, which occurs because of preexisting antibodies in the recipient. “In the early days of xenotransplantation, when you did the transplant, the organ would immediately turn black because of the rejection,” he says. “Through genetic engineering, we have overcome hyperacute rejection.” But other phases of rejection can occur months or even years after transplant, in what are called early and late rejection. A group at the University of Maryland has performed two pig heart transplants into live patients, who survived for about two months, providing information on early rejection. But there is no data yet about late rejection.
Despite the remaining challenges, Moazami remains confident that xenotransplantation will be successful, perhaps as soon as another decade. “These are not hills that we can’t climb over, but we are collecting the data and developing the science so that someday we can do it,” he says. “The fact of the matter is that the technology exists to be able to engineer these pig organs, to be able to make xenotransplantation one day a clinical reality.”
American Scientist Comments and Discussion
To discuss our articles or comment on them, please share them and tag American Scientist on social media platforms. Here are links to our profiles on Twitter, Facebook, and LinkedIn.
If we re-share your post, we will moderate comments/discussion following our comments policy.