From Research to Reality
By Katherine Elizabeth Willmore
To understand her son’s birth defect, a mother makes an emotional and scientific journey
To understand her son’s birth defect, a mother makes an emotional and scientific journey

DOI: 10.1511/2011.92.358
Just over two years ago, I had my first child, Max. My entire pregnancy was magically boring. Both baby and I were in perfect health—until the last month, when we learned that Max was breech. No big deal, my husband Eric and I figured. We’d just get in touch with the local doctor who is known for his ability to “spin” babies—to turn them so that they are facing downward toward the birth canal. Then I got a call from my midwife. My most recent ultrasound had revealed some problems; I had to have more tests right away.

SPL/Photo Researchers
At the hospital, the doctor told me that my amniotic fluid was extremely low and that Max would have to make his debut a little early. We were unable to turn Max into position, and my hopes of natural childbirth were dashed. I was scheduled to get a Caesarean section in two days. Not sure how to prepare, my husband and I spent the evening before the arrival of our first child doing our taxes and then celebrating with sushi (just veggie rolls for me).
The very idea of a C-section freaked me out. Needles make me weak in the knees, and the thought of being awake while a doctor made a large cut in my abdomen didn’t sit well with me. Luckily, I was so excited about meeting our baby that I could push my fears aside. And the operation went well. Max came out shivering and crying and, in the eyes of his parents at least, absolutely beautiful. My husband, Max and the midwife left the operating room while the doctors closed me up. As I was wheeled back into our room, my midwife came to my side. “Max has a cleft palate,” she said. This would be shocking news for anyone. But the kicker is that, as part of my Ph.D. thesis, I had conducted research on cleft palate. My eloquent response was, “You’re shittin’ me.” As it turns out, though, people don’t joke about developmental disorders in newborns.
My initial shock shifted, over the first few days of Max’s life, to oppressive guilt. Mixed in with these emotions were feelings of grief. Even in the moment, I could feel that this grief was over-the-top—we had been spared many other, more serious problems—so I did my best to hide the feelings from others and from myself. Throughout the pregnancy we had wondered about the usual things. Is it a boy or a girl? Will he be tall like his dad or short like me? Will he be colicky? In fact, the ills of a colicky newborn were the only negative thoughts I allowed myself. So when I learned that Max had a cleft palate, I mourned the loss of the “perfect” baby I had naively expected. But my overriding emotion was worry, a constant, niggling fear that something horrible would happen to Max because of the cleft. Will he be able to feed okay? Can he breathe all right? Are there other developmental problems that we’re unaware of? We spent the first few months just waiting for the other shoe to drop.
As it turns out, we’ve been very fortunate. Max is thriving and there have been no unforeseen problems. Two days before his first birthday he had surgery to repair his cleft, and the entire ordeal went swimmingly. The doctors did an amazing job, and one would never guess that Max once had a problem with his palate. Still, I often find myself wondering, what are the odds that someone who has done research on a disorder would have a child afflicted with that disorder?
Now that the worry has subsided, the tears have dried, and the guilt has been sufficiently suppressed, I’m able to look at Max’s developmental mishap through scientist-colored glasses. I’d forgotten how fascinating the intricacies of development can be. Considering the wild, choreographed steps required for proper facial development, I find it surprising that there aren’t more missteps.
Figures adapted by Tom Dunne from The Developing Human: Clinically Oriented Embryology, by Keith L. Moore and T. V. N. Persaud, pages 180–181 and 191, copyright Elsevier 2008.
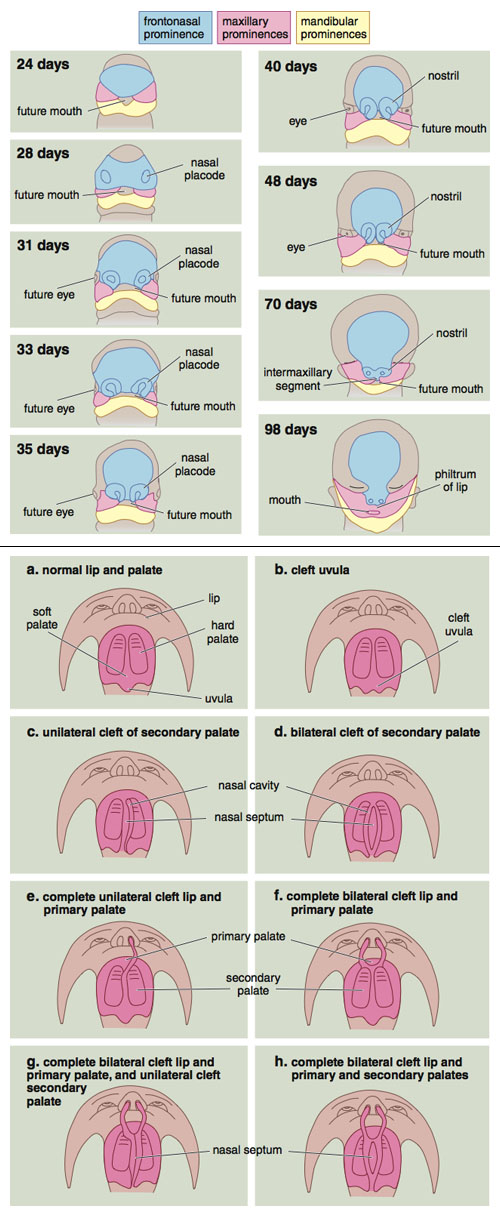
The variety of possible facial clefts is mind boggling. A child can be born with a cleft lip, a cleft palate or both. I discovered soon after Max’s birth that when most people hear “cleft,” they seem to imagine only a cleft lip (what was once more commonly called a harelip), and particularly one that involves a large, gaping hole. Before Max’s surgery, when I told people that he had a cleft palate, the response was a nearly universal “You would never know.” This was a comfort—because we weren’t usually dangling our kid upside down for people to see inside his mouth, his cleft was not normally on display.
A cleft lip is characterized, as the name suggests, by a separation of the upper lip. This can be a small groove in the upper lip, or a large gap that extends from the nostril through the lip and the bone of the upper jaw where the two front teeth are housed. Depending on the severity of the cleft, the infant’s ability to suckle may be impaired, and speech and dental complications may arise.
Cleft palate, on the other hand, involves a gap in the roof of the mouth. To understand where a cleft lip ends and a cleft palate begins, feel the roof of your mouth with your tongue. Just behind your front teeth there is a small ridge. This marks approximately where the primary palate, found at the front of the mouth, meets with the secondary palate, found at the back of the mouth. When a cleft lip affects the bone of the upper jaw, it extends only as far as this ridge and disrupts only the primary palate. In contrast, a cleft palate affects only the secondary palate, behind the ridge. It can extend from the uvula (the dangly thing at the back of your mouth) all the way to this ridge; Max had this type of cleft. It can involve just a small cleft in the uvula, a small slit along the middle of the palate, or a gap that extends the entire width and depth of the mouth. In all cases, a cleft palate disrupts the usual separation between the mouth and the nasal passages. The result is an inability to suckle, as well as problems with speech. More entertaining (or distressing, depending on your point of view) consequences are extreme snoring and the ability to squeeze food through your nose—a fine party trick.
To add to the complexity, the different clefts can mix and match like sweater-set coordinates. The seemingly endless combinations can lead to the impression that facial clefts occur randomly. In fact, there are few structures involved in facial clefting, and with an understanding of the development of the face, the variety becomes predictable.
Facial development for a human embryo begins early in the fourth week of development, when five facial prominences appear around the area that will become the mouth. These swellings of embryonic tissues act as growth centers of the face. I like to think of them as blobs of Play-Doh—each a pliable mass that can be pushed and pulled into a variety of shapes. Above the future mouth are two maxillary prominences, which form the upper jaw and the cheek regions of the face. Sandwiched between them is the frontonasal prominence, which forms the forehead and nose. Below the opening of the future mouth lie the paired mandibular prominences that will fuse to form the lower jaw.
The first parts of the face to develop are the lower lip and jaw, which are essentially formed by the tenth week of development. The two mandibular prominences grow toward each other until they meet at what will be the center of the chin and lower lip, at which point they fuse. Our nostrils, which begin to develop at the end of the fourth week, start off as paired, oval-shaped thickenings of the frontonasal prominence, called nasal placodes. The outer margins of the placodes grow faster than the insides do. To visualize this, imagine an inflatable swimming pool. As you blow air into the pool, the sides rise as they take on most of the air, with very little air going to the bottom of the pool. Similarly, the fast growth of the outer margins of our nasal placodes forms the sides of our nostrils.
Meanwhile, the maxillary prominences are growing rapidly. They push against the nasal portion of the frontonasal prominence, causing the primitive nostrils to move closer to each other. At the end of the sixth week, the maxillary prominences start to fuse with the outer parts of the nostrils, joining the cheek regions with the sides of the nose. Then they ooze underneath the frontonasal prominence and finally meet at the midline underneath the primitive nose. Between the seventh and tenth weeks, the middle portions of the two nostrils fuse with each other and with the maxillary prominences below. These fusion events form separate nostrils with a single septum between, creating continuity between the nose, cheeks, upper jaw and lip.
Palate development takes place between the sixth and twelfth weeks, but the period from the end of the sixth week to the beginning of the ninth is most critical. The primary palate, located at the front of the mouth, begins to develop early in the sixth week. When the nostrils fuse together to form a single septum in the middle, a portion of the frontonasal prominence gets squished downwards. This portion, which now lies below the nose and between the maxillary prominences, is called the intermaxillary segment. The little divot between your nose and mouth, called the philtrum, is part of this structure, as is the primary palate, which includes the bone that houses your upper two front teeth.
Development of the secondary palate begins around the same time, but it is a more complicated process. Initially, the tissue that will form the secondary palate hangs vertically from each maxillary prominence, on either side of the tongue. These dangling bits of tissue are called the palatal shelves. As the lower jaw elongates with growth, the tongue is able to move forward and flatten so that it lies below the palatal shelves. Then, during the seventh and eighth weeks, one of the most incredible developmental events occurs: Over just a few hours, the palatal shelves actually elevate from a vertical to a horizontal position. Once the shelves are in place, they continue to grow until they meet in the middle of what will become the roof of the mouth, where they fuse with each other and with the primary palate in front.
All these acts of fusion require timed coordination of cell movement, cell death and cell growth. To understand the process, it may be easier to think of what it would look like for a part of the body that we can see. Imagine that your index and middle fingers are going to fuse along their sides. First, the skin that lies between them must break down. The cells that make up this skin die, leaving the tissue within each finger free to intermingle. The tissue of each finger then grows toward and into that of the other. Finally, skin grows over the site of fusion, creating one large finger. This scenario may read like science fiction, but the essential processes themselves are what create our very real-world faces, fusing the different elements of the palate and the rest of our facial structures.
Understanding facial development reveals why facial clefts vary so widely: Clefts occur where fusion is disrupted. Failure of one of the maxillary prominences to fuse with the intermaxillary segment, for example, causes a unilateral cleft lip; failure of both to fuse results in a bilateral cleft lip. Failure of the palatal shelves to elevate creates a cleft secondary palate, like the one our son had, but has no effect on the primary palate or lips. In other cases, one shelf elevates and the other remains vertical, leading to a unilateral cleft palate. And in others, both shelves elevate but do not grow enough to meet at the midline, causing a somewhat less severe cleft. Even if the shelves do elevate properly, failure of the skin between them to break down can disrupt the fusion process, creating a cleft that might only become noticeable when the child starts to speak.
What remains unknown are the factors that cause fusion failure in the first place. Syndromic clefts arise as part of a syndrome in which other structures are also disrupted. More than 400 syndromes that involve facial clefting have been reported. There is often a clear association between the syndrome and specific genes, but the full role that most genes play is not usually known. And the source of the problem is often not the genes associated with the palate. Rather, the mutated genes encode generic developmental processes that help build a variety of structures, including our lungs, teeth, hair and limbs, along with the palate. The generic nature of these processes is what links the often disparate symptoms associated with craniofacial disorders such as Apert syndrome, Crouzon syndrome, Treacher-Collins syndrome and velocardiofacial syndrome. And the same mutation can affect people differently, depending on the rest of the genome and their environmental circumstances. One mutation could be responsible for a minor divot in the top of the upper lip in one individual and a complete bilateral cleft lip in another. Scientists are working to learn how these genes interact with the rest of the genome and with the environment, but current understanding of such interactions is still poor.
At least with syndromic clefts we have a starting point in the search for causes. But the majority of facial clefts appear on their own, with no other symptoms and no known associated mutations. These isolated clefts make up approximately 70 percent of cleft-lip cases and 50 percent of cleft-palate cases. Although our understanding of the mechanics of face and palate development is strong, the large number of factors that contribute to development, and the even greater number of interactions between these factors, keep the underlying cause of most cleft cases a mystery.
Given the coordination of so many complex processes required for proper development, I marvel that most children are born without birth defects. I realize how fortunate our family is that Max was born with just a cleft palate. And I have learned that the odds of having a child with cleft palate are not that low: About every two and a half minutes, somewhere in the world a child is born with a facial cleft.
Revisiting the scientific literature on facial clefting has been a cathartic experience for me. Looking at Max’s cleft from a biological perspective forced me to be objective and confirmed what my family, friends and health practitioners had been telling me. There was no way to predict that Max would have a cleft palate, it wasn’t my fault, and there is no reason to fear having another child. The veil of guilt has lifted a little further—that is, until I find myself laughing at old photographs of Max in his high chair with mashed peas streaming out of his nose.
Click "American Scientist" to access home page
American Scientist Comments and Discussion
To discuss our articles or comment on them, please share them and tag American Scientist on social media platforms. Here are links to our profiles on Twitter, Facebook, and LinkedIn.
If we re-share your post, we will moderate comments/discussion following our comments policy.