Changing Policies on COVID-19 Transmission
By Katie L. Burke
A Q&A with Linsey Marr
A Q&A with Linsey Marr

Despite its top-notch scientific institutions, the United States fared especially poorly during the COVID-19 pandemic. There were many missed opportunities that led to such an epic tragedy. One that has loomed especially large has been confusion around airborne spread of the virus. Precautions such as improving indoor air quality or wearing masks were ignored or downplayed until far too late. Linsey Marr, an engineer who studies aerosols at Virginia Tech, suddenly found her expertise needed in 2020 in the rapidly unfolding public health emergency—and yet she and others in her field were not included among the regulatory scientists working on the guidelines for the World Health Organization and U.S. Centers for Disease Control and Prevention (CDC). Digital features editor Katie L. Burke spoke with Marr about how she and her colleagues worked for years to change policies based on faulty ideas about transmission of the coronavirus. This interview has been edited for length and clarity.

Photo by Peter Means courtesy of Virginia Tech
How did you start working on airborne transmission?
Before 2009, I’d mainly been studying outdoor air pollution, particle emissions from vehicles. I became interested in airborne transmission when my son started day care in 2009. As with all kids who start day care, he got sick a lot. The day care center had what we consider good hygiene practices.
I started reading about how flus and colds spread. I was surprised to learn that at a mechanistic level, the way I think about particle pollution spreading through the air, we didn’t actually know how viruses were getting from one person to another. There was the idea that they were coming out in these large, wet droplets that people would cough or sneeze onto each other. But frankly there wasn’t a lot of evidence for that. They were missing out on the fact that people also release much tinier droplets, aerosol particles you can’t see, that could potentially contain a virus. The first thing we did was collect particles from the air in a day care center, in the university health center, and on airplanes. We knew what size they were. In half our samples, we found the flu virus in these very tiny particles—not near a sick person, but just floating around in the air.
When the pandemic hit, what were you thinking about as you were hearing the first news about the virus?
In the outbreak of SARS 1 in 2003 and 2004, it had been pretty well established that that virus was transmitted through an airborne route. When I first heard about severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), my first assumption was, well, there’s no reason why this wouldn’t be too. Then, I was seeing the rapid spread in China, and then the locking down. I was seeing photos of health care workers in China in the hospitals wearing full protective gear. I knew you wouldn’t go to the trouble of wearing that unless the virus was very transmissible. Those things tipped me off that SARS-CoV-2 was probably airborne too. In January 2020, I was thinking, yeah, this virus is probably airborne.
At that time, I also knew that the traditional thinking in medical and public health circles was that this virus would be transmitted by large droplets [as opposed to airborne aerosols] when people are close to each other, coughing on each other within six feet. There was a New York Times article published at the end of January, about six things that are important for understanding the spread of this virus. One of the questions was, How far does the virus travel? This article said this one doesn’t travel very far, unlike measles and some others that can travel hundreds of feet or more. I thought that was totally wrong. I replied to the New York Times in a tweet and said, “I don’t believe this. Why do people think this?”
Seeing things evolve throughout February 2020, it was clear that the U.S. medical and public health communities were doubling down on this idea that the virus was spreading just through these large droplets—over a distance no greater than six feet—and that we needed to worry about contaminated surfaces. I had my doubts. What clinched it for me was the Skagit Valley Chorale outbreak in early March 2020 in Washington State.
What was it about that outbreak that confirmed your suspicions that the coronavirus could be airborne?
It was the fact that the people going into that practice, the rehearsal, knew that this virus was there. They took some precautions. They avoided shaking hands. They spaced themselves out. Nevertheless, more than 50 people became infected at that one rehearsal. Even if they had shared food, or let’s say everyone had touched the same doorknob, the idea that that doorknob or whatever object could become contaminated by one person, and then you could have 50 people come by and subsequently touch that same object, and there’s still virus on it even after the first few people touch it? I just found that unbelievable.
Can you clarify the technical meaning of the terms droplet, aerosol, and airborne?
In the traditional definitions of disease transmission, the word droplet refers to things that are larger than 5 or 10 microns. These are assumed to travel kind of ballistically, following a certain trajectory as they come out of one person’s mouth or nose, fly through the air, and land in someone else’s eyes or nose or mouth, or land on a surface and contaminate it. That was thought to be the major way that colds and flu were transmitted. Then there are also aerosols, defined to be smaller than that cutoff. Those were thought to transmit mainly at long distances. Diseases such as measles and tuberculosis were acknowledged to be transmitted by aerosols, to be airborne.
But the big blind spot medical researchers had in those definitions is that when you have these very small particles, they can transmit across a long distance or a close distance. When people are close to one another, they’re even more likely to be exposed to these small particles.
Why was this idea that colds, flus, and SARS-CoV-2 spread by droplets rather than aerosols so entrenched? What was keeping people from acknowledging aerosols?
I don’t know. I think a lot of the ideas about disease transmission were observations of who gets sick. After an outbreak, researchers would look for so-called close contacts, people who were in close proximity to the infected person. Then, they would find that these close contacts became sick. The thing is, because of the way their contact tracing was defined, they didn’t really look at other people who were maybe in the room, but not closely associated with the infected person. They weren’t looking for it, and so they didn’t see it.
In January 2020, I was thinking, yeah, this virus is probably airborne.
Another potential reason is that a lot of understanding of infectious disease transmission grew out of what happens in hospitals. Modern hospitals are pretty well ventilated. Under those conditions, you’re less likely to see airborne transmission. If people are wearing surgical masks, they wouldn’t completely block this route of transmission, but would help reduce it. And researchers and regulatory scientists could see these large, wet, visible droplets. It’s easy to understand that those could carry and transmit virus. But for every one of those, there are hundreds of these tiny particles that you can’t see. These scientists didn’t know those smaller particles were there.
Medical researchers and MDs are experts on what’s happening when a pathogen is inside your body. I have no expertise in that. Once it gets into your body, I don’t know what happens. But if you’re thinking about what happens to that pathogen when it’s outside your body in the indoor or outdoor environment, I would argue that an environmental engineer or aerosol scientist has the right expertise to understand what is happening with that pathogen when it’s moving around among people.
It seems like dividing transmission into this binary [droplet versus aerosol] doesn’t make sense. I understand that from a policy perspective one often has to create categories and thresholds. But in this case, it ended up being confusing.
The way that the infection prevention and control community defined transmission was very binary. A disease was either transmitted by droplets or it was airborne. But in reality, when people are in close proximity, transmission could be via either route, large droplets or aerosol particles.
Before the pandemic, were you already working to change policies around airborne transmission? Or did that only happen once the pandemic arrived?
I had brought it up a few times. Other people who have expertise in this area also had brought it up but were ignored. I would say we were ridiculed, even, in some cases. We’re outsiders to the field. The thought was, “Oh, what do these people know? They have no idea that this is how it’s been defined for 50 years.” It was kind of like shouting into the void. Obviously, this topic became much more critical during the pandemic, because if we continued to focus on droplets—staying six feet away from one another and wiping down surfaces—I didn’t think we were going to control the disease very well.
An environmental engineer or aerosol scientist has the right expertise to understand what is happening when a pathogen is moving around among people.
Lidia Morawska in Australia is also an expert in this field, and she pulled together a group of researchers worldwide who have expertise in how pathogens move around in the environment—most of us not MDs. She arranged a meeting with the WHO in early April 2020. I don’t think they wanted to hear what we had to say. So, Morawska led efforts to publish a public letter to the WHO, saying, “We’re pretty sure this is what’s happening. You need to update your science so that we can control the spread better.” We had 239 cosigners on this letter, which was published in July 2020 in Clinical Infectious Diseases.
It kind of took the WHO by surprise. They responded by acknowledging that airborne transmission can happen in special circumstances—for example, when there are what they called “aerosol-generating medical procedures” taking place in health care settings, such as intubating someone. They just were not aware that when people breathe and talk, they generate aerosols—actually more than are generated through these medical procedures.
Walk me through what happened over the course of the next couple of years, until policies really did start changing.
In August of 2020, there was a National Academies of Science, Engineering, and Medicine workshop on airborne transmission of SARS-CoV-2. Various experts spoke at that workshop and presented evidence for airborne transmission. It was a very strong case at that point. Coming out of that workshop, Kim Prather, who’s a professor at University of California, San Diego, led a commentary in Science, called “Airborne Transmission of SARS-CoV-2.” We summarized the findings from the workshop in 300 words, which was published in October of 2020, and we let the CDC know that the publication was coming. In response, they temporarily changed their website information about transmission, but then it was changed back. This was weird.
After that, the next major event was that in the following spring of 2021, there were three papers by various groups about airborne transmission, each published within the same week in major medical journals—JAMA, the Lancet, and the British Medical Journal. At that point, the message really broke through, because these papers were published in highly respected medical journals. The medical community could no longer just ignore it. One doesn’t tend to pay attention to journals outside of one’s field. Soon after that, the CDC adjusted their website and put airborne transmission at the top of their guide on how the coronavirus is transmitted. Later that year, the WHO finally changed its scientific information as well. But they didn’t really publicize that change very well. It’s almost like they tried to do it under the radar, on December 23, the day before Christmas Eve.
Where did that resistance at the CDC or WHO come from?
I don’t know for sure. My impression is that there was a lot of concern about acknowledging airborne transmission because of the implications it would have for health care. In hospitals, if you say a disease is airborne it means you need respirators for all health care workers and airborne infection isolation rooms, meaning negative pressure rooms, for patients. That’s very expensive. A lot of hospitals just don’t have the capacity to do that for the number of patients that they were getting. And so the WHO did not want, I think, to put hospitals in a bad position, where they would not be able to provide the care that is expected if you have an “airborne” disease.
I now know that the CDC will not make a recommendation for materials if they are not available. Early on in the pandemic the CDC was not going to recommend respirators for people even if they wanted to, because N-95s were simply not available. We didn’t even have enough for health care workers at that point; they were sterilizing and reusing them.
I imagine, just seeing how the world works, that liability would be a big issue too, for health care workers who got sick on the job. If the airborne transmission were acknowledged, then the employer is responsible for providing respiratory protection for their employees.
How long did it take to change policy around airborne transmission?
In 2021 the CDC reorganized its guidance for the public about transmission and started talking about ventilation. The WHO had a really nice document on ventilation as well. It was during 2021 that they finally started providing guidance about ventilation and placing less emphasis on wiping down surfaces. But there was still a lot of emphasis on handwashing. That’s still the message that a lot of the public remembers: six feet and handwashing.
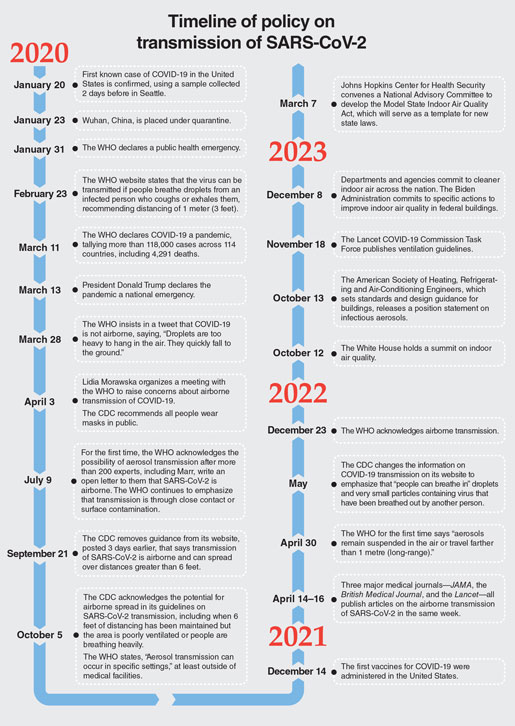
Then there were, of course, all kinds of political issues about masking. The guidance gradually changed, but people had already heard the initial messages, and I think there wasn’t a big campaign to help people recognize the change in guidance. By the time the guidance changed, masks had been politically poisoned. Eventually in 2021 the White House Office of Science and Technology Policy tried to promote awareness of ventilation and virus transmission.
How did you feel going through this?
I was exhausted, because I was working a lot of hours for two years. I was doing 10 media interviews a week for a couple of years, on top of everything else I was trying to do. It was very frustrating to have to fight so hard to try to educate people. The public was open to it, but the medical community—they had learned something in a textbook. It’s hard to change your beliefs when you’ve learned something one way.
What have you learned from this process of policy change?
I’ve learned that it is messy. It’s slow. It’s hard to get it right the first time. There are so many different factors and stakeholders. It’s not just about following the science, but you have to consider feasibility, the public’s willingness to hear a message. If you say something that’s not achievable, people aren’t going to bother. There are economic considerations. There are political considerations. I realized at one point that maybe a mask mandate is actually counterproductive, because it makes people hate masks so much, or the enforcement is so onerous. There were fights over this, shootings over this. At that point I realized, well, ideally everyone would wear masks, but in our current social and political setting maybe mandating that is not the best thing.
I realized that you have to get the message to decision-makers or key players in the venues that they use and respect. You have to find an ally at some point who’s in that community. In terms of getting into the medical journals, it was important to find an ally who was an MD.
What are some common misconceptions you encounter about airborne transmission of COVID, even today?
A lot of people still think that handwashing and distancing are the most important things they can do. But really they need to be thinking about the air we’re breathing. That’s harder, because we don’t see it. We’re not used to thinking about that. The message for that came out much later, when people were fatigued. It wasn’t promoted as much.
For institutions who want to make sure they’re following good guidelines for preventing the spread of COVID-19 now, where can they go for examples?
The U.S. Environmental Protection Agency has good information about buildings and ventilation. It’s called the Clean Air and Buildings Challenge. The CDC has some good information now also about masks and the importance of good ventilation. The WHO has a good worksheet on ventilation. The Harvard Healthy Schools and Healthy Buildings program also has some excellent guidance documents available.
What are you working on now?
My lab works on understanding how viruses survive in the environment, in droplets or aerosols. (See “Optimal Conditions for Viral Transmission,” April 3, 2020.) We’ve wrapped up our last paper on SARS-CoV-2. We aerosolized virus, pulled it through different kinds of masks, and looked at how much would transfer to your fingers if you were to touch it. We used artificial skin. We didn’t find any infectious virus that transferred to skin. So this idea of touching a contaminated mask maybe isn’t such a big concern.
Then we have a big interdisciplinary project called Mitigate Flu, looking at transmission in day care centers in Michigan and then also using some animal models to study transmission under controlled conditions. We’re trying to develop better methods of detecting a virus in the air and on surfaces.
Then we have another project, doing what’s called a human challenge study, where we will deliberately infect people with the flu virus, and then put them in certain situations with other people who aren’t infected to see how many people get infected.
And finally, I have a student who’s looking at antibiotic resistance, how bacteria and their genes are transported through the air.
Click "American Scientist" to access home page
American Scientist Comments and Discussion
To discuss our articles or comment on them, please share them and tag American Scientist on social media platforms. Here are links to our profiles on Twitter, Facebook, and LinkedIn.
If we re-share your post, we will moderate comments/discussion following our comments policy.